I recently attended a two day workshop that was all about understanding functional neurological disorders that was in a word, mind-blowing (ok maybe that’s two words). It was hosted by two fantastically experienced and engaging clinicians, Helen Clarke (Speech & Language Therapist) and Dr Rachel Dean (Clinical Psychologist). In the aftermath I’m still trying to collect my thoughts and digest what I have learnt. I truly feel it has changed my practice forever. Anyway! To help me process and digest I thought I would do a blog all around the mechanistic model of FND (Functional Neurological Disorder) that much of the workshop was based around.
I have written about FND previously, but here is a quick re-cap of what the condition actually is. Functional Neurological Disorder (FND) is a complex condition where individuals experience neurological symptoms—like seizures, paralysis, or sensory disturbances—that cannot be explained by traditional medical or neurological conditions. The symptoms are very real and can be as debilitating as those caused by other neurological diseases, but they do not have a clear “organic” cause, making FND a challenging condition to diagnose and treat.
The Mind-Body Connection in FND
One of the most intriguing aspects of FND is the interplay between the mind and the body. Historically, medicine has often separated these two, treating physical and psychological conditions independently. However, FND highlights the limitations of this approach, as patients frequently exhibit symptoms that straddle both realms. This necessitates a more integrated approach to diagnosis and treatment.
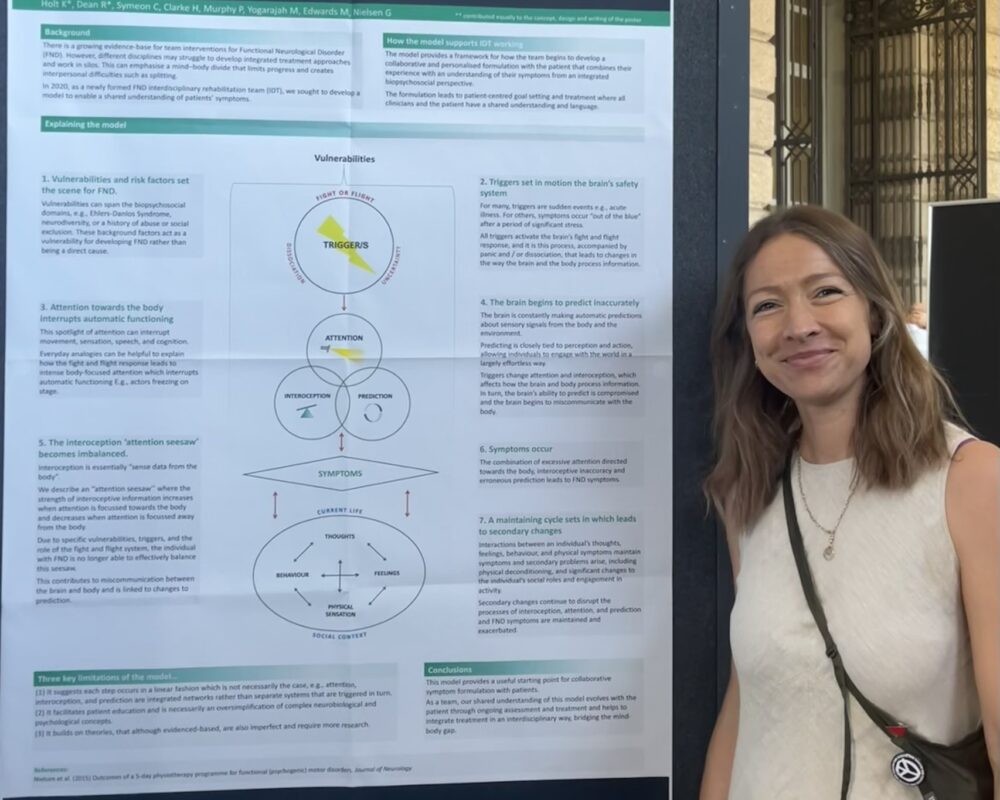
The model highlights the interplay between vulnerabilities for developing FND e.g. trauma, stress and how a change to attention from “auto-pilot” to increased attentional focus can shift the body into a dysfunctional response. For example, a person who has had a severe choking episode on chicken, then becomes hyperaware of their oral movements and how they are swallowing food. This can then cause a seemingly impaired swallow function as this attentional switch takes the person from swallowing on “auto-pilot” as they have done for most of their life to being acutely aware and worried about their swallowing. These symptoms then become somewhat of a “viscious cycle” that can be very difficult to break without appropriate interventions. This TEDX video by Lorimer Moseley does a much better job of summarising it than myself – check it out here. Although it is centered around pain, the premise is very similar.
The Interdisciplinary Team Model for FND
Holt et al. propose an interdisciplinary team model for managing FND, which aims to bridge the gap between the mind and body. This model brings together specialists from various fields to provide a comprehensive, patient-centered approach to care.
Key Components of the Interdisciplinary Team Model
- Neurology: Neurologists play a crucial role in the initial diagnosis and management of FND. They help rule out other neurological conditions and collaborate with other team members to develop a treatment plan.
- Psychiatry/Psychology: Mental health professionals address the psychological aspects of FND. They work on understanding the patient’s emotional and cognitive processes, which might contribute to or exacerbate symptoms. Therapies such as cognitive-behavioral therapy (CBT) can be particularly effective.
- Physiotherapy: Physiotherapists help patients regain movement and function. They design personalised exercise programs that consider both the physical and psychological aspects of FND.
- Occupational Therapy: Occupational therapists focus on improving patients’ ability to perform daily activities. They teach strategies to manage symptoms and enhance quality of life.
- Speech and Language Therapy: For patients with communication or swallowing difficulties, speech and language therapists provide targeted interventions to improve communication and swallowing functions.
- Social Work: Social workers assist with the broader social and environmental factors affecting patients. They provide support with navigating healthcare systems, accessing community resources, and managing family dynamics.
Benefits of the Interdisciplinary Approach
The interdisciplinary team model proposed by Holt et al. offers several benefits:
- Holistic Care: By addressing both the physical and psychological components of FND, this approach ensures that patients receive comprehensive care tailored to their unique needs.
- Collaborative Treatment Plans: Regular team meetings allow for the integration of different perspectives, leading to more effective and cohesive treatment plans.
- Patient Empowerment: Patients are encouraged to participate actively in their care, fostering a sense of control and empowerment, which is crucial for managing chronic conditions.
- Improved Outcomes: Studies suggest that patients receiving interdisciplinary care for FND experience better outcomes in terms of symptom reduction and quality of life improvements compared to those receiving traditional care.
Moving Forward
The model proposed by Holt et al. represents a significant step forward in the treatment of FND. It underscores the importance of breaking down the barriers between different medical disciplines to provide patient-centered care that addresses the complexities of FND.
As healthcare systems continue to evolve, adopting such interdisciplinary approaches could pave the way for more effective management of not only FND but also other conditions that lie at the intersection of the mind and body. This holistic approach promises to improve patient outcomes and enhance the overall quality of care.
Functional Neurological Disorder may be challenging, but with innovative models like the one proposed by Holt et al., there is hope for more effective and compassionate treatment strategies that bridge the gap between the mind and body.
If you or a loved one are struggling with FND, then don’t hesitate to contact us here to see if we can support you at all.




